Case Study
Despite Advances in Technology, Retained Surgical Items Still Occur
Description
A patient required additional surgery to remove a retained foreign item.
Key Lessons
- Every team member has a role in ensuring accurate surgical item counts.
- Effective communication is crucial for patient safety to avoid any misunderstanding about items on the surgical field.
- Leverage interdisciplinary teams to review data and enhance existing protocols, policies, and procedures to prevent retained surgical items.
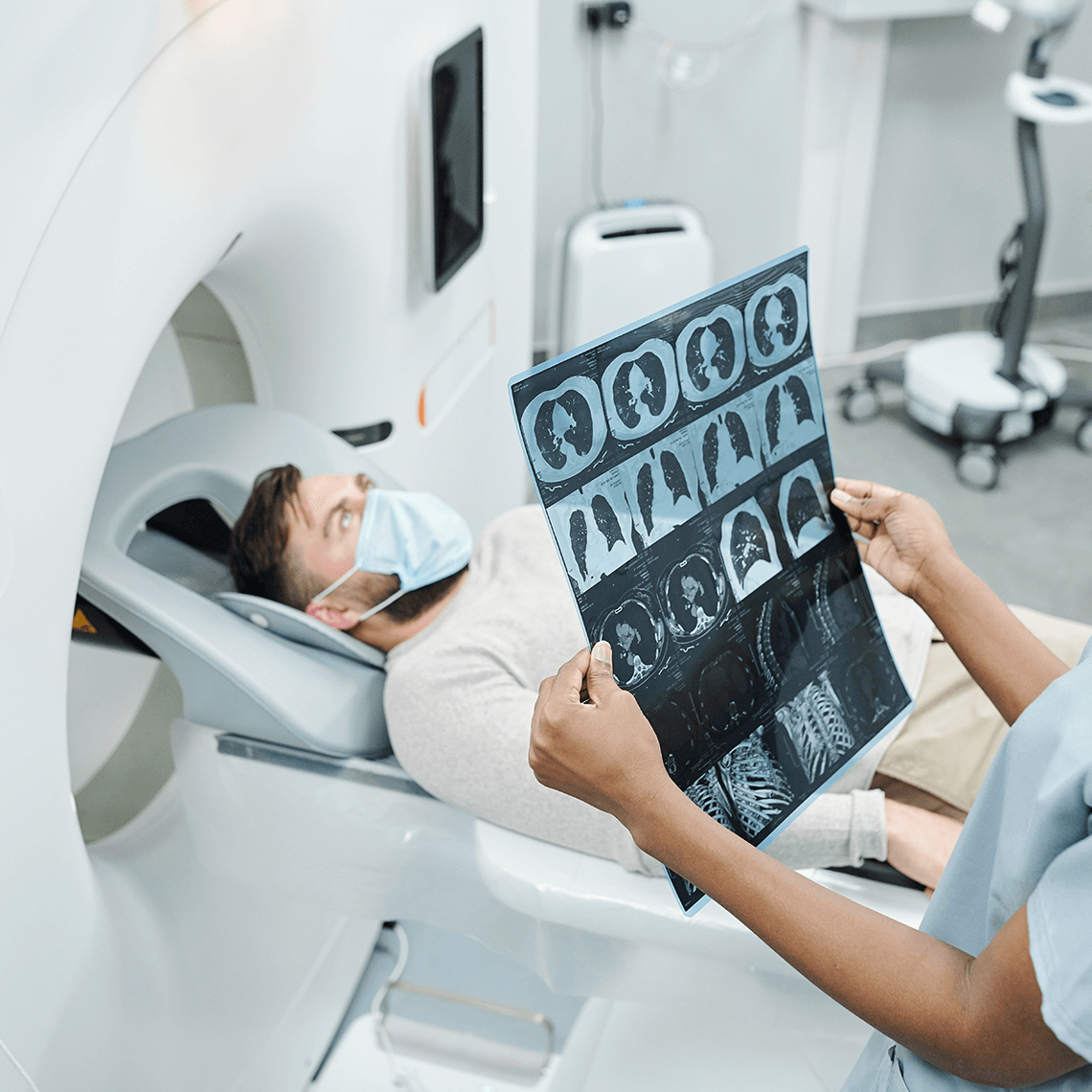
Clinical Sequence
A patient with symptomatic coronary artery disease underwent a coronary artery bypass graft surgery. They did well intraoperatively and had a normal post-operative course. Prior to discharge, an X-ray showed an opacity in the upper left lung field. The finding was communicated to the care team with a plan to repeat the chest X-ray at the patient’s follow-up appointment. A few weeks after discharge, the patient complained of pain in their chest. A CT scan identified a retained surgical item; the patient then returned to the operating room where the item was identified and removed.
Allegation
A retained surgical item resulted in the need for additional surgery.
Analysis
Policies and protocols were not followed in this case.
The case review revealed that the retained surgical item was not recorded, documented, or tracked in the surgical item count.
The item did not have any markings that could be easily identified on an X-ray or with radiofrequency identification technology.
At the end of the procedure, the retained surgical item was not identified during the closing count nor with a radiofrequency wand.
Disposition
Case settled in the low range (<$99,999).
Discussion Questions
- What policies and procedures do you have in place to prevent retained surgical items?
- How do you record and track surgical items that do not have radiofrequency markings or tags?
- How do you engage the entire intraoperative team to effectively communicate and identify when unique surgical approaches or equipment are used?
- Does the whole surgical team participate in time-outs, briefings, and debriefings?
- Do you speak up when you have a patient safety concern?
Resources
- Understanding Retained Surgical Items (RSI): Importance, Prevention, and AORN Guidelines
- Guidance to Reduce the Risk of Retained Surgical Items
- Quick Safety Issue 20: Strategies to prevent URFOs (Updated May 2022)
- The Joint Commission: Sentinel Event Data 2024 Annual Review
- Safety Net Podcast: Alert on Surgical Items Left Behind in Patients
- Strategies for Patient Safety: No Surgical Items Left Behind
See More MPL Cases
Medication Mix-up Contributes to Patient’s Death
Retaliation Allegation after Mental Health Leave
Incidental Does Not Mean Insignificant